CommentsPUBLIC HEATH-The CDC is now telling us to wear “Do it yourself” aka: DIY masks when we are out in public.
(Photo courtesy of FACEBOOK – screen shot of video of Mayor Eric Garcetti working on face shields for the COVID – 19 response.)
“CDC continues to study the spread and effects of the novel coronavirus across the United States. We now know from recent studies that a significant portion of individuals with coronavirus lack symptoms (“asymptomatic”) and that even those who eventually develop symptoms (“pre-symptomatic”) can transmit the virus to others before showing symptoms. This means that the virus can spread between people interacting in close proximity—for example, speaking, coughing, or sneezing—even if those people are not exhibiting symptoms. In light of this new evidence, CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.
It is critical to emphasize that maintaining 6-feet social distancing remains important to slowing the spread of the virus. CDC is additionally advising the use of simple cloth face coverings to slow the spread of the virus and help people who may have the virus and do not know it from transmitting it to others. Cloth face coverings fashioned from household items or made at home from common materials at low cost can be used as an additional, voluntary public health measure.
The cloth face coverings recommended are not surgical masks or N-95 respirators. Those are critical supplies that must continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance.”
We are told by our elected officials here in California to “Stay at Home,” “Shelter in Place,” and to only go out for essential needs. Now the message seems to be for Seniors and those who are Immune Compromised not even to go to the grocery store or to the drug store.
April 2, 2020: Email from Mayor Eric Garcetti:

“Whenever there is a new step we can take to protect our communities from the spread of COVID-19, I want to make sure you know about it as soon as possible.
Los Angeles is a leader in responding to this global crisis, and that’s why I want to share the latest guidance from public health experts on how you can help protect yourself and those around you from infection. As we learn more about this virus, we will continue to update our guidance so we don’t just flatten the curve, but get ahead of it.
We are recommending that all Angelenos wear face coverings in public.
We have issued new guidance to LA residents on the importance of wearing face coverings in public. The California Department of Public Health has also shared public guidance on the use of face coverings.
Early data suggests that many who are infected with COVID-19 do not have symptoms, which is why everyone should wear cloth face coverings when leaving the house for essential activities. However, a face covering is not a substitute for other critical measures — most importantly, staying home as much as possible, washing hands frequently, and practicing safe physical distancing in all settings.”

As I take this message from an email from Mayor Garcetti, it asks the reader to watch the video above.
Mayor Garcetti – are you aware that the reader cannot watch this video without logging into a FACEBOOK account? I want you to know that I know a lot of people who are not on FACEBOOK or social media including members of my former Neighborhood Council. So your message may not be reaching your target audience.
This is continued from Mayor Garcetti’s email:
“Please note: a face covering is not the same as a mask.
N95 and other medical-grade masks are reserved for medical workers like doctors and nurses — and using the medical masks that they need could cost someone their life.
The public should use non-medical face coverings, such as bandanas or scarves, or make your own from cloth. And they’re only effective together with personal hygiene measures like frequent hand washing, as well as safe physical distancing. Your face coverings should be washed after each use.
We know L.A. is a creative city, and I’m sure Angelenos will lead the nation in coming up with innovative ways to make face coverings. Please share great ideas on how you made your own unique face covering on social media with the hashtag #LAProtects.
The bottom line is simple: everyone should stay home as much as possible, and if you must go out for an essential errand, you should have your face covered.
Please share these updates. Every person you tell could be a life saved.
You can find more information and resources at Coronavirus.LACity.org, and make sure you’re signed up for notifications from the City of L.A. at NotifyLA.org.
Thank you for doing your part to help stop the spread of COVID-19 and protect your family, friends, neighbors, and community from this virus.
Stay healthy, stay safe, and stay home.
Eric Garcetti
Your Mayor”
A ROYAL SNAFU! DIY MASKS!
After I wrote my article, “THE CORONAVIRUS AKA: COVID-19 (SARS-CoV-2): What We Are Learning About Our Lack of Preparedness,” I received an email from a member of the City family. This person questioned my recommendation for the respirators with a valve system.
City personnel, it appears, are being told that the respirators with valves like the P95 I recommended are for use in construction. Yes that is true, but with a shortage of respirators – which are, in my opinion, superior in protection to a face mask, it was my understanding that the government was turning to all aspects of every available industry to provide whatever facial protection that was available to the first responders.
This was my response back to that individual:
The information below is directly from this page link above. I have highlighted and bolded things in red for emphasis because of what I consider to be confusion in our elected officials, employees, and even members of some public health agencies who may not be familiar with the differences between masks for medical personnel and respirators.
“How can health care workers be protected from SARS?
Most transmission of SARS to health care workers appears to have occurred after close contact with SARS infected individuals. CDC has therefore issued interim infection control recommendations for health care and other institutional settings (see Updated Interim Domestic Infection Control Guidance in the Health-Care and Community Settings for Patients with Suspected SARS, Interim Domestic Guidance on the Use of Respirators to Prevent Transmission of SARS, and Transport of Patients with Suspected SARS.)
These guides recommend that health care workers entering the room of a SARS patient and medical transport workers transporting a patient with suspected SARS use the following:
-
Standard precautions (e.g., hand hygiene)
-
Contact precautions (e.g., use of gown and gloves for contact with the patient or their environment)
-
Eye protection for all patient contact
-
A respirator that is at least as protective as an N-95 respirator approved by the National Institute for Occupational Safety and Health (NIOSH)
Infectious material deposited on personal protective equipment may cause it to become a vehicle for direct or indirect transmission. Therefore, care is needed when removing personal protective equipment to avoid contaminating skin, clothing, and mucous membranes. Standard procedures for removal of personal protective equipment that minimize the potential for self-contamination should be developed based on the equipment used, and healthcare and transport workers should be trained in these procedures. Hand hygiene should be performed following the removal of personal protective equipment.
What is a respirator and what is a NIOSH-approved N-95 respirator?
A respirator is a personal protective device that is worn on the face, covers at least the nose and mouth, and is used to reduce the wearer’s risk of inhaling hazardous airborne particles (including dust particles and infectious agents), gases, or vapors. The many types of respirators available include (1) particulate respirators, which filter out airborne particles; (2) “gas masks,” which filter out chemicals and gases; (3) airline respirators, which use compressed air from a remote source; and (4) self-contained breathing apparatus, which include their own air supply. The category of particulate respirator can be further divided into (1) disposable or filtering facepiece respirators, where the entire respirator is discarded when it becomes unsuitable for further use due to excessive resistance, sorbent exhaustion, or physical damage; (2) reusable or elastomeric respirators, where the facepiece is cleaned and reused but the filter cartridges are discarded and replaced when they become unsuitable for further use; and (3) powered air purifying respirators (PAPRs), where a battery-powered blower moves the air flow through the filters.
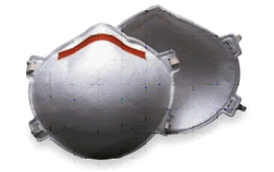
An N-95 respirator is one of nine types of disposable particulate respirators.
Particulate respirators are also known as “air-purifying respirators” because they protect by filtering particles out of the air as you breathe. These respirators protect only against particles—not gases or vapors. Since airborne biological agents such as bacteria or viruses are particles, they can be filtered by particulate respirators.
Respirators that filter out at least 95% of airborne particles during “worse case” testing using a “most-penetrating” sized particle are given a 95 rating. Those that filter out at least 99% receive a “99” rating. And those that filter at least 99.97% (essentially 100%) receive a “100” rating.
Respirators in this family are rated as N, R, or P for protection against oils. This rating is important in industry because some industrial oils can degrade the filter performance so it doesn’t filter properly.* Respirators are rated “N,” if they are Not resistant to oil, “R” if somewhat Resistant to oil, and “P” if strongly resistant (oil Proof). Thus, there are nine types of disposable particulate respirators:
-
N-95, N-99, and N-100;
-
R-95, R-99, and R-100;
-
P-95, P-99, and P-100
NIOSH uses very high standards to test and approve respirators for occupational uses. NIOSH-approved disposable respirators are marked with the manufacturer’s name, the part number (P/N), the protection provided by the filter (e.g., N-95), and “NIOSH.” This information is printed on the facepiece, exhalation valve cover, or head straps. View a listing of all NIOSH-approved disposable respirators.If a disposable respirator does not have these markings and does not appear on one of these lists, it has not been certified by NIOSH. NIOSH also maintains a database of all NIOSH- approved respirators regardless of respirator type on the Certified Equipment List.
More detailed respirator information has been published by NIOSH, CDC and by the Occupational Safety and Health Administration external icon (OSHA).
*The SARS virus has a “shell” composed of lipids, which are fats and oils. However, the amount of fat and oil in these tiny virus particles is extremely low and is not enough to affect the filter in the N-series respirator. Thus the N-series respirators such as N-95 will protect against SARS exposure.
Can health care workers use respirators other than N-95 to protect against SARS?
Yes, workers can wear any of the types of particulate respirators for protection against SARS—if they are NIOSH-approved and if they have been properly fit-tested and maintained. All of the NIOSH-approved particulate respirators protect workers against SARS as effectively as the N-95 respirators.
A respirator will work only if it is used correctly. Thus, the key elements for respiratory protection are fit-testing and training of each worker in the use, maintenance, and care of the respirator.
NIOSH considers each of the nine types of disposable particulate respirators to have similar fit characteristics. Therefore, when a worker is caring for or transporting SARS patients, having a NIOSH-approved respirator that fits well is much more important than whether the respirator is an N-95 or one of the other eight types of disposable particulate respirators.
In health care settings, the use of respirators by workers is regulated under the Occupational Safety and Health Administration (OSHA) standard for respiratory protection. The OSHA standard sets requirements for the fit-testing of respirators to ensure a proper seal between the respirator’s sealing surface and the wearer’s face. The OSHA standard also contains requirements for determining that workers can use respirators safely, for training and educating employees in the proper use of respirators, and for maintaining respirators properly. NOTE: Fit-testing and the other OSHA-required procedures are absolutely essential to assure that the respirator will provide the wearer with required protection. View detailed information on respiratory programs external icon, including fit test procedures.
Why are N-95 respirators most often recommended for SARS?
The CDC Guidelines for Isolation Precautions in Hospitals recommends that health care workers protect themselves from any disease spread through the air (airborne transmission) by wearing a respirator at least as protective as a fit-tested N-95 respirator.† These guidelines were written before SARS was discovered, but they have been used to protect against other airborne diseases such as tuberculosis.
†Although N-95 respirators are sold outside the United States, other particulate respirators are also available. If you live in another country, your country may have its own standards for particulate respirators. The particulate respirators may have different names than those certified by NIOSH in the United States. If these respirators pass testing programs comparable to those used for N-95 respirators, they should protect against SARS as well as the N-95 respirators.
Can I use a respirator with an exhalation valve?
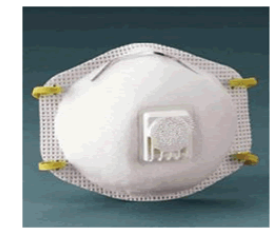
Usually, yes. An exhalation valve reduces excessive dampness and warmth in the mask from exhaled breath.
The valve opens to release exhaled breath and closes during inhalation so that inhaled air comes through the filter. Health care workers may wear respirators with exhalation valves unless the patient has a medical condition (such as an open wound) for which a health care worker would normally wear a surgical mask to protect the patient. Similarly, respirators with exhalation valves should not be placed on a patient to contain droplets and prevent spread of infectious particles; surgical masks are adequate for this purpose.
How often do disposable respirators need to be replaced?
Once worn in the presence of a SARS patient, the respirator should be considered potentially contaminated with infectious material and touching the outside of the device should be avoided. Upon leaving the patient’s room, the disposable respirator should be removed and discarded, followed by hand hygiene.
If a sufficient supply of respirators is not available, healthcare facilities may consider reuse as long as the device has not been obviously soiled or damaged (e.g., creased or torn). Data on reuse of respirators for SARS are not available. Reuse may increase the potential for contamination; however, this risk must be balanced against the need to fully provide respiratory protection for healthcare personnel.
If N-95 disposable respirators are reused for contact with SARS patients, implement a procedure for safer reuse to prevent contamination through contact with infectious droplets on the outside of the respirator.
Consider wearing a loose-fitting barrier that does not interfere with fit or seal (e.g., surgical mask, face shield) over the respirator.
-
Remove the barrier upon leaving the patient’s room and perform hand hygiene. Surgical masks should be discarded; face shields should be cleaned and disinfected.
-
Remove the respirator and either hang it in a designated area or place it in a bag. (Consider labeling respirators with a user’s name before use to prevent reuse by another individual.)
-
Use care when placing a used respirator on the face to ensure proper fit for respiratory protection and to avoid contact with infectious material that may be present on the outside of the mask.
-
Perform hand hygiene after replacing the respirator on the face.
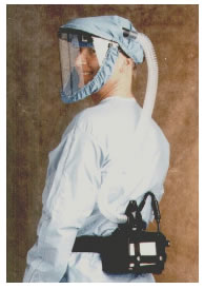
My hospital uses powered air-purifying respirators (PAPRs). Will they protect me from SARS?
Yes. PAPRs use HEPA filters (high-efficiency particulate air filters), which are as efficient as P-100 filters and will protect against SARS. PAPRs provide a higher level of protection than disposable respirators. Health care facilities in some SARS-affected areas have used higher levels of respiratory protection, including PAPRs, for persons present during aerosol-generating medical procedures such as bronchoscopy on SARS patients. When PAPRs are used, their reusable elements should be cleaned and disinfected after use and the filters replaced in accordance with manufacturer’s recommendations. All used filters should be considered potentially contaminated with infectious material and must be safely discarded.
Do surgical masks provide protection against SARS?
Surgical masks are not designed for use as particulate respirators and do not provide as much protection as an N-95 respirator. Most surgical masks do not effectively filter small particles from air and do not prevent leakage around the edge of the mask when the user inhales.
If surgical masks do not protect against airborne diseases, why are surgical masks suggested for use against SARS when no N-95 respirators are available?
Surgical masks are recommended only as a last resort for health care and medical transport workers exposed to SARS patients when no NIOSH-approved respirator equivalent to or greater than the N-95 is available. SARS appears to be transmitted mainly through direct contact with infectious materials (including large respiratory particles), and surgical masks will provide barrier protection against droplets that are considered to be the primary route of SARS transmission. However, surgical masks may not adequately protect against aerosol or airborne particles, primarily because they do not effectively filter small particles from the air, they allow leakage around the mask, and they cannot be fit tested. Because scientists cannot currently rule out the spread of SARS through the air, CDC recommends a NIOSH-approved respirator equivalent to or greater than the N-95.
Surgical masks may also be placed on patients with communicable conditions like SARS to contain respiratory droplets and prevent spread of infectious particles.
I don’t work with SARS patients. Should I wear a respirator while I am at work or in public?
Both CDC and the World Health Organization (WHO) recommend respirator use for the following workers only:
-
health care workers entering the room of a patient with SARS
-
medical transport workers transporting patients with suspected SARS
Respirators are not routinely needed (by staff or visitors) in other parts of hospitals or other health care facilities where there is no direct contact with patients.
Outside the health care and medical transport settings, CDC does not recommend the routine use of respirators. Most people who develop SARS become infected through contact with other people who are ill with SARS? not by breathing contaminated air. If a person does contact the SARS virus, it is most likely to be on a surface such as a doorknob. The best protection from SARS in public places, (including workplaces other than health care and medical transport settings) is to wash your hands frequently and avoid touching your eyes or nose.”
GUIDANCE FOR FACE PROTECTION AND PERSONAL SAFETY IN INCONSISTENT AND RAPIDLY CHANGING!
Resources:
· CDC: How to Protect Yourself & Others.
· CDC: Use of Cloth Face Coverings to Help Slow the Spread of COVID-19.
3M Science applied to life – Worker Health and Safety.
At the bottom of this page, there is an excellent video: “Mask vs. Respirator. what is the difference?”

· Dr. John Campbell: “To mask or not to mask”
Dr. Campbell reviews the current literature and explains it in an easy to understand way. In this video, he explains that the Coronavirus actually can extend from a cough or a sneeze much further than the six-foot distance that we are being told to keep. It justifies the “Stay at Home” advice as well as the need for those workers who work in the stores or as delivery personnel to have the appropriate respiratory and glove coverage; why we should be using good hand washing hygiene, and why these personnel and the public should be wearing the appropriate face coverings and disposable gloves when shopping in my opinion.
· “Turbulent Gas Clouds and Respiratory Pathogen Emissions Potential Implications for Reducing Transmission of COVID-19”; Lydia Bourouiba, PhD1, March 26, 2020.
My Conclusions:
In my opinion, there will be no return in the near future to the “normal” as we remember it. Even if we get a brief respite later this summer from the virus, it will most likely reemerge later in the fall until we get a vaccine.
This will mean that the “new normal” will require everyone to have personal protective equipment like hospital grade masks or respirators as well as disposable gloves.
It will mean that we should expect that our school kids may be home again next fall for online teaching. It will mean more and more services will be handled remotely.
We may need to remember the days when we had “gas rationing lines” around 1973, and we may want to consider days of the week that people can shop based upon their last name as we did with license plates of cars in the 1970s. We may need to be forced to ration food because some are stockpiling it while others have difficulty finding it.
Our government at all levels has known about the potential for contagious diseases that can be transmitted from humans to humans or animals to humans for a very long time.
According to news sources, the State of California had a stockpile of respirators and ventilators and other emergency equipment that it chose not to keep stockpiled. See: “California once had mobile hospitals and a ventilator stockpile. But it dismantled them.”
From the best of my understanding, this virus is not going away soon. A vaccine is at least a year or more away. Then we will need to be able to mass produce it and see if it is effective against the virus. We need to build up “herd immunity” to this virus. And there will be those who are against vaccines who will fight their use.
Our government must make protection from viral and bacterial infection preparedness equal to preparedness for wildfires, earthquakes, and the impacts of climate change. How we are going to pay for this level of preparedness? I don’t know. There seems to be a desire in the private sector to partner with our government in this effort related to the Coronavirus.
Thanks to our elected officials, and our local, state, and federal employees who have to continue to work during this crisis.
Thanks to our medical professionals at all levels – doctors, nurses, respiratory technicians, x-ray techicians, laboratory technicians, patient care workers, and even the laundry and custodians – we could not have health care without all of you.
Thanks to our First Responders – LAPD, LAFD, Sheriffs, and LA County Fire Fighters for your assistance in this fight.
We need to thank not only our grocery stores and pharmacies, and sites such as Amazon, but also everyone from their management -- the stock personnel, the cashiers, the janitors, the shoppers, and the truck drivers.
And finally, we cannot forget our farmers. Who would be providing our food if it were not for our farmers? As someone who lived on a farm, it’s now planting season where I grew up. I hope that this virus does not impact our farmers and the workers they need to plant and harvest crops and care for the animals from which we get meat, eggs, and dairy.
Thank you. Be safe. Be Healthy.
(Chris Rowe, a former health care employee who has worked at Northridge Hospital, Tarzana Medical Center, and West Hills Hospital has a B.S. in Health Education. She is a 42-year resident of West Hills. She has written for the Los Angeles Daily News, RonKayeLA.org; OurLA.org; and CityWatch. She has a blog on the USC/ Annenberg Center for Health Journalism website and can be reached at [email protected]) Edited for CityWatch by Linda Abrams.